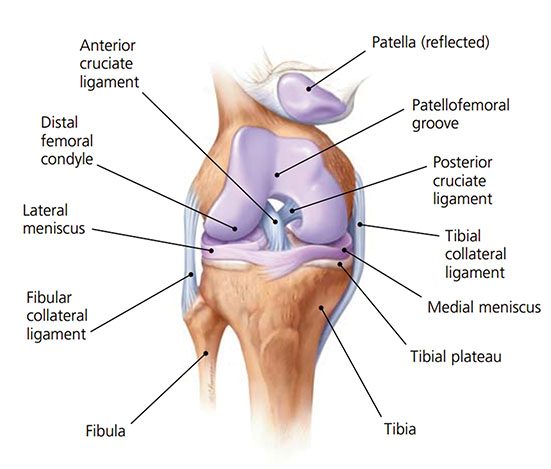
Knee pain is a common condition experienced by people of all ages and levels of activity. When discussing knee pain terms such as ‘Retro Patella pain’, ‘Patella Femoral dysfunction’, ‘Medial Compartment Syndrome’, ‘Chondromalacia Patella’, or ‘Iliotibial Band Friction Syndrome’, are often used – however these terms are simply descriptions of different types of knee pain.
Generally ‘knee pain’ can be medial, lateral or anterior depending on the foot mechanics and the biomechanical anomalies that a patient presents with.
Biomechanical Aetiology
There are many contributing factors including: an increased Q-angle (the angle formed between the longitudinal axis of the femur, representing the line of pull of the Quadricep muscle and a line representing the pull of the patella tendon), genu valgum and genu varum, muscle tightening through the gastrocnemius, Iliotibial band and VMOs, hyper-extension of the knee and tibial torsion and rotation.
When assessing and treating knee pain, it is important to remember that the knee sits in between the hip and the foot, therefore there is often a relationship between the hip and knee, and foot and knee.
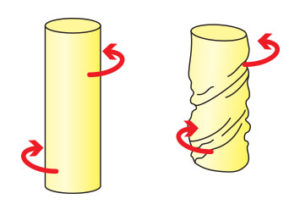
If knee pain is idiopathic, pronation and supination (or a combination of both) may be the underlying cause. Michaud (1997) states that for every 1° of pronation, the tibia internally rotates 1° in turn affecting the knee joint as it takes the stress generated by tibial rotation. Internal or external tibial rotation can cause medial displacement of the patella-femoral path and may encourage lateral or medial displacement of the patella as the external hip rotator muscles or adductors tighten as a compensation for pronation, supination and external and internal tibial torsion.
Pain can be experienced on the lateral collateral ligaments when the foot strike angle is in a supinated position or there is a forefoot valgus anomaly > 10° which encourages the foot to strike laterally to gain ground contact and this in turn places pressure upon the lateral aspect of the knee.
If the patient strikes laterally and then at mid stance quickly pronates in the gait cycle the patient will often experience anterior knee pain as the patella tendon moves both laterally and then medially ; this situation is one which occurs often with patients that exhibit a forefoot valgus deformity < 10° as this will allow pronation to occur during mid stance phase of gait.
Internal tibial rotation is a contributing factor in causing medial collateral strain to the ligament structures that wrap around the medial aspect of the knee and lower leg. External tibial rotation can place additional stress on the lateral aspect of the knee compartment. A complicating factor can be the introduction of a forefoot valgus deformity and or external or internal torsion of the tibial shaft which will illicit a compensatory response in the soft tissues to correct the out toed or in toed Malleolar position to the so called ‘normal’ position as out lined by Root (1977) and discussed in Clinical Biomechanics, Volume 20, Issue 4 (2005), p443-450 Xiang Liua, Wangdo Kima, Burkhard Drerupb, Arjandas Mahadevc].
Symptoms
Knee pain can be experienced laterally, medially or anteriorly. It may be experience as a dull ache or as a sharp grabbing pain. Often with sports people, the pain does not occur until sometime into their training regime.
Anterior knee pain sufferers often say that the pain is all over the knee and so it is important to assess for a forefoot deformity as part of the assessment procedure.
Treatment
Orthotics should be prescribed and worn to assist in realigning the foot to the Neutral Calcaneal Stance Position, in turn restoring the knee joint to the correct alignment, thus preventing further wear and tear of the joint. If a forefoot valgus deformity is identified during assessment, and the patient is experiencing lateral or anterior knee pain, an ICB forefoot valgus addition can be applied to the orthotic to assist in treatment.
Additional Treatment
- Dry needling can be used to the point of pain.
- Stretches and strengthening should be done wearing correctly aligned orthotics to gain the best results from the program.
Head Office
Kirrawee NSW 2232
AUSTRALIA